Lipostatic hypothesis
For the course duration, the article is closed to outside editing. Of course you can always leave comments on the discussion page. The anticipated date of course completion is 01 April 2012. One month after that date at the latest, this notice shall be removed. Besides, many other Citizendium articles welcome your collaboration! |
In 1953, Kennedy [1] proposed what became known as the lipostatic hyothesis. Specifically, he postulated the existence, in the hypothalamus, of a centre that was sensitive to the concentration of metabolites in the circulation, which prevented "an overall surplus of energy intake over expenditure."
Introduction
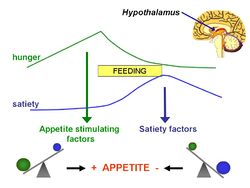
The lipostatic hypothesis describes the feedback mechanisms between adipose tissue deposition and hypothalamic signalling, in order to sustain 'lipostasis'. Lipostasis is achieved through the modulation and balancing of energy intake and expenditure to prevent an individual 'getting fat'. For the brain to know when their is too much adipose tissue building up, a signalling hormone must be released from the adipose tissue to signal to the brain that a satiation signal must be released in order to stop the individual from eating. In 1994, it was discovered that this hormone released from adipose tissue, and critical in regulating the size of the body fat depot, was coded for by the ob gene and is known as leptin[2].
What is leptin?
Leptin is a adipocite derived hormone that circulates in the blood in proportion to whole body adipose tissue mass. In other words, except for ob/ob individuals, the more adipose tissue an individual contains, the greater the amount of leptin they have circulating in their blood. Leptin is a hydrophobic hormone and can therefore through endocytosis cross the blood-brain barrier and act on specific leptin receptors which are mainly located in the ventromedial hypothalamic nucleus (VMN) and arcuate nucleus (ARC). The leptin signal transmits information about the size of body fat depots, binds to leptin receptors in the VMN, causing the production of POMC, which acts on further secondary neurones leading to the release of satiation signals.
Leptin was discovered as a product of the ob gene and its role in regulating food intake was identified through ob/ob knockout mice. These ob deficient mice could not produce leptin and therefore had no means of starting the feedback mechanism, as there was no signalling to the VMN and ARC of excess adipose tissue. Due to this, there is no anorexigenic response and the ob/ob mice keeps on eating due to a lack of satiation feeling. Another mutation that further supported leptins role in energy balance came from db/db deficient mice. These mice expressed leptin insensitive receptors and therefore, even though their adipose tissue produced leptin in abundance, the lack of leptin sensitive receptors also meant that there was no complete signal to the brain of excess adipose tissue.
Interestingly, leptin treatment of these two different mutant mice led to drastically different results. The ob/ob mice, when treated with leptin over time, lost a vast amount of weight as leptin elicits the anorexigenic response that the mouse could not provide before. The db/db mice however had no weight reduction from the introduction of leptin, as their receptors remained insensitive to the hormone.
Hypothalamic leptin signaling
Leptin receptor mediated hypothalamic signaling involves multiple pathways. The JAK2/cytosolic signal transducer and activator of transcription protein 3 (STAT3) pathway plays an important role, although the JAK2-Phosphotidylinosital 3 kinase (PI3K) pathway has also shown to be important. With respect to the JAK2/STAT3 pathway, leptin binding to the long form of the leptin receptor (Ob-Rb) initiates tyrosine phosphorylation of Ob-Rb by JAK2. Phosphorylated leptin receptor then recruits STAT3 that is activated through phosphorylation by JAK2. The activated STAT3 proteins dimerize and translocate to the nucleus where they bind DNA and initiate gene transcription. Suppresser of cytokine signaling 3 (SOCS-3) and phosphotyrosine phosphotase 1B (PTP1B) are two known negative regulators of leptin signaling following Ob-Rb activation through a mechanism of negative feedback. The JAK2/STAT3 pathway is believed to be essential for mediating leptin's effects on homeostatic energy regulation.
In the hypothalamus leptin binds to leptin receptors in the ARC and PVN which then activates the POMC/CART neurones leading to the synthesis of α-MSH which is a potent inhibitor of appetite. Experimetnal rodent models have shown that injection of α-MSH directly into the brain of these animals strongly inhibits the feeding response。 As well as this leptin has shown to inhibit the NPY/AgRP neurones which have been shown through animal models to be potent stimulators of appetite. There is also a communication system between these two sets of NPY/AgRP and POMC/CART neurones- activation os one set of neurones inactivates the other set of neurones and vice versa.
Parabolis evidence
In the 1950s it was hypothesized that there was a message from the adipose tissues signalling to the brain, telling the brain how fat you are. Different parabolis experiments (involv the surgical joining of two circulations of mice from a common single strain}Different experiments were undertaken involving: diet induced obese mice, ob/ob (leptin deficient) mice and db/db (no leptin receptors) mice, to try and determine if there was a factor in the blood that influenced fat and body weight.
Experiments i)Diet induced obese mouse + normal lean mouse = weight loss in normal mouse ii) Normal weight mouse + ob/ob obese mouse = weight loss in obese mouse iii)Normal weight mouse + db/db obese mouse = weight loss and death in normal mouse
These experiments show that there is a factor in the blood which is now known to be leptin which is released from the adipose tissues into the blood stream and acts on the hypothalamus. In experiment i) the diet induced obese mouse is leptin insensitive (but has high levels of leptin in the circulation), therefore parabolis of the two mice means that the levels of leptin are increased in the circulation leading to weightloss in the normal mouse. In experiment ii) the ob/ob mouse has a single gene defect which means that it cannot synthesize leptin, therefore the parabolis of the mice means that the levels of leptin are increased in the circulation, this leptin can act on the hypothalamus of the ob/ob mouse leading to weight loss. In Experiment iii) the db/db mouse has mutant leptein receptors, but still synthesizes extremely high levels of leptin. The parabolis means that the levels of leptin in the circulation are significantly increased, the leptin acts on the hypothalamus of the normal weight mouse, leading to significant weight loss and eventual death.
As experiment ii) shows in patients with a single gene mutation that prevents the synthesis of leptin, leptin therapy has been shown to significantly improve obesity disease. Mutations in the receoptor as far less well understood and characterized and thus far therapys used to treat these defects have had inconsistent results. Mutations in the leptin receptor (db/db) are much more common than mutations in leptin synthesis (ob/ob) therefore future work needs to be done to further charcterize the pathways involved in receptor signalling to ebanle the development of therapies to threat this disease.