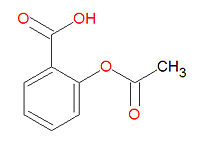
Aspirin
Aspirin, or acetylsalicylic acid, is the "prototypical analgesic used in the treatment of mild to moderate pain. It has anti-inflammatory and antipyretic properties and acts as an inhibitor of cyclooxygenase which results in the inhibition of the biosynthesis of prostaglandins. Specifically, it inactivates the enzyme prostaglandin synthase by acetylating its terminal amino group. Aspirin also inhibits platelet aggregation and is used in the prevention of arterial and venous thrombosis."[1] Aspirin is a non-steroidal anti-inflammatory agent, often abbreviated as NSAID.
Aspirin resistance may cause susceptibility to cardiovascular morbidity.[2]
Aspirin resistance
Individuals in whom platelet function assays demonstrate resistance to aspirin are less likely to have cardiovascular protection from aspirin or other antiplatelet treatments.accompanied by rhinorrhea[3] As many as 28% of patients are resistant to aspirin.[4]
Apparent resistance may be due to inadequate patient compliance, especially in the setting of polypharmacy.[5]
Asthma, nasal polyps, and aspirin intolerance
Among patients with asthma, 10% to 20% may have bronchoconstriction accompanied by rhinorrhea.[6]
Effectiveness
Cancer
Aspirin may prevent death from cancer.[7]
Adverse effects
Gastrointestinal hemorrhage
The gastrointestinal tract is the most common site of bleeding from aspirin.[8]
Intracranial hemorrhage
This may especially occur if the systolic blood pressure is above 130 or 145 mm Hg.[9]
External links
The most up-to-date information about Aspirin and other drugs can be found at the following sites.
- Aspirin - FDA approved drug information (drug label) from DailyMed (U.S. National Library of Medicine).
- Aspirin - Drug information for consumers from MedlinePlus (U.S. National Library of Medicine).
- Aspirin - Detailed information from DrugBank.
References
- ↑ Anonymous (2024), Aspirin (English). Medical Subject Headings. U.S. National Library of Medicine.
- ↑ Krasopoulos, George et al. 2008. “Aspirin "resistance" and risk of cardiovascular morbidity: systematic review and meta-analysis.” BMJ 336(7637):195-198. http://www.bmj.com/cgi/content/full/336/7637/195
- ↑ Krasopoulos G, Brister SJ, Beattie WS, Buchanan MR (2008). "Aspirin "resistance" and risk of cardiovascular morbidity: systematic review and meta-analysis". BMJ 336 (7637): 195–8. DOI:10.1136/bmj.39430.529549.BE. PMID 18202034. Research Blogging.
- ↑ Online Mendelian Inheritance in Man, OMIM®. Johns Hopkins University, Baltimore, MD. MIM Number: 608223. World Wide Web URL: http://omim.org/.
- ↑ Pignatelli P, Di Santo S, Barillà F, Gaudio C, Violi F (October 2008). "Multiple anti-atherosclerotic treatments impair aspirin compliance: effects on aspirin resistance". J. Thromb. Haemost. 6 (10): 1832–4. DOI:10.1111/j.1538-7836.2008.03122.x. PMID 18680540. Research Blogging.
- ↑ Online Mendelian Inheritance in Man, OMIM®. Johns Hopkins University, Baltimore, MD. MIM Number: 208550. World Wide Web URL: http://omim.org/.
- ↑ Rothwell PM, Fowkes FG, Belch JF, Ogawa H, Warlow CP, Meade TW (2010). "Effect of daily aspirin on long-term risk of death due to cancer: analysis of individual patient data from randomised trials.". Lancet. DOI:10.1016/S0140-6736(10)62110-1. PMID 21144578. Research Blogging.
- ↑ Berger JS, Roncaglioni MC, Avanzini F, Pangrazzi I, Tognoni G, Brown DL (January 2006). "Aspirin for the primary prevention of cardiovascular events in women and men: a sex-specific meta-analysis of randomized controlled trials". JAMA 295 (3): 306–13. DOI:10.1001/jama.295.3.306. PMID 16418466. Research Blogging.
- ↑ Meade TW, Brennan PJ (July 2000). "Determination of who may derive most benefit from aspirin in primary prevention: subgroup results from a randomised controlled trial". BMJ 321 (7252): 13–7. PMID 10875825. PMC 27417. [e]