Intrauterine device
An intrauterine device (IUD) is a birth control option that is 99+% effective in preventing pregnancy, and if inserted within five days of unprotected sex, it still works[1]. An IUD is a 1- to 2-inch piece of flexible plastic installed by a doctor into a woman's uterus, where it remains until removed (possibly years later) and prevents implantation of a fertilized egg. An IUD can be used by a woman even if she cannot tolerate the side effects of pills and patches. As of 2023, there are 5 brands of IUDs that are FDA-approved for use in the United States:[2]
- Paragard
- Mirena
- Kyleena
- Liletta
- Skyla
The insertion process
An IUD is inserted by a medical practitioner during an office visit. Typically, the woman is unsedated and she may experience brief discomfort (typically a sharp, quick, pinching sensation like a very bad menstrual cramp) during the insertion, but if properly positioned, any discomfort should recede very quickly. The woman is usually not sedated because, if there is persistent pain, this means the device is not in a good position and needs to be removed. After insertion, the woman may experience minor bleeding or discharge for a day or two, after which everything should feel completely normal. Ideally, a woman should find a very experienced and compassionate practitioner for the insertion; inexperienced practitioners are more likely to cause the woman discomfort during insertion. To be nearly painless, the practitioner must perform the insertion quickly and with confidence in the amount of pressure they apply during the insertion--hence, experience counts.
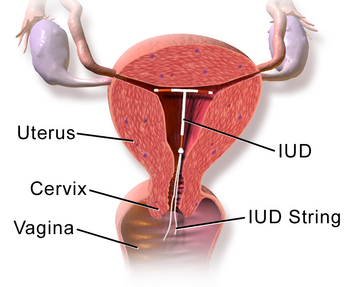
Once an IUD is inserted successfully, the woman is supposed to be given training on how to check daily on the IUD's proper positioning. This is done by the woman feeling for the string at the mouth of the cervix with her fingertips. If the woman follows the recommendations for regularly checking the IUD's position, risks of side effects from the IUD are quite low. However, sometimes in the past, practitioners were negligent in not instructing women properly, and also, some women neglect to follow the recommended checkup guidelines, opening up the possibility of side effects.
Remainder of the past article, which is being revised
Clinical practice guidelines address management.[3] Barrier methods rely on consistent, technically correct use to be effective, so their typical failure rates in practice are higher than they would be with perfect compliance. By contrast, the IUD has similar rates of failure for both typical and perfect use. First year failure rates are less than 1% for the copper T 380A IUD and 2% for the progesterone-releasing IUD.[4]
Unlike cervical caps and diaphragms, which are placed into the vagina by the user, the IUD is placed into the hollow uterus by the health care provider. The inside of the uterus is an internal body cavity, and is not accessible except by a health care provider. Placement of the IUD usually is performed in the office or clinic, and requires the dilation of the normal opening of the cervix (cervical os). The procedure is uncomfortable for the woman, and there is a risk of contaminating the interior of the womb. In most IUDs, there is a string that exits the uterus through the cervical os and can be felt in the vagina. Although placing an IUD is a medical procedure rather than a surgical procedure, it is a skilled procedure that must be carried out in a clean environment.
IUDs are spontaneously expelled from the uterus in many cases, and once expelled, no longer provide protection. The rate of expulsion is related to the position of insertion, and is lowest when an experienced and skillful clinician places the device high in the fundus of the uterus. Expulsions are most common during the first year after insertion, and the rate of pregnancy decreases after this first year. With some devices, the cumulative risk of pregnancy over a decade is less than 2%. With long-term placement, the annual incidence of side effects such as excessive bleeding or cramping also decreases.
"Contemporary IUDs rival tubal sterilisation in efficacy and are much safer than previously thought."[5] However true that may be, IUDs have been associated with a higher rate of fallopian tube occlusion and resultant infertility. Many gynecologists recommend the use of IUDs as being nearly ideal for older women, especially for those women who have a low risk of contracting a sexually transmitted infection and those who have substantially finished childbearing. Cite error: Closing </ref> missing for <ref> tag. Copper-containing IUDs appear not to entail significant risk of copper toxicity, as neither serum nor urine copper levels increase, suggesting non-absorption of copper from intrauterine fluid.[6]
Progesterone-containing IUDs do not appear to be spermicidal. Although the overall rate of pregnancy is much lower in women with these IUDs than in control groups not using contraception, the rate of ectopic pregnancy is higher in the progesterone-containing IUD group than in the 'no-contraceptive' group. The reduced rate of pregnancy is therefore most likely due to reduced implantation of fertilized ova rather than reduced fertilization of ova. In other words, progesterone-containing IUDs appear to work mostly by preventing normal pregnancy from ever being established in the uterus rather than by preventing conception.
IUD insertion as an emergency contraceptive
Emergency contraception is the use of a drug or device to prevent pregnancy after unprotected intercourse.[7] Placement of an IUD is one form of emergency contraception. It is generally recommended that IUDs be avoided in women who are at high risk of sexually transmitted infections; in women with these infections, especially Chlamydia, there is a much higher rate of pelvic inflammatory disease with an onset soon after insertion of the IUD. Although this disease is treatable with antibiotics, it results in a significant rate of complications, including permanent infertility. Because IUDs are contraindicated as an emergency contraceptive when there is a significant risk of a sexually transmitted disease, this is not a method recommended for emergency contraception after rape.
Side effects and complications
Bleeding is the main reason that women who seek to have IUDs removed do so, either because of prolonged, excessive or inter-menstrual bleeding (bleeding between periods). Perforation of the device through the uterine wall does occur, and although most often is not a serious complication, rarely can cause an acute abdomen from peritonitis that requires emergency surgery. The small risk of pelvic inflammatory disease associated with IUDs is limited to the first few weeks after insertion. [8]
Mirena, the levonorgestrel-releasing intrauterine system may or may not contribute to decreased bone mineral density. The two negative studies are small and limited to measurements of bone-mineral density at the forearm.[9][10] The positive study is a single case report.[11]
Pregnancy rates after IUD removal
In previous decades, the common wisdom among health scientists and women using contraceptives was that IUDs were generally associated with a high risk of permanent sterility from fallopian tube obstruction caused by pelvic inflammatory disease. However, the risk of pelvic inflammatory disease with the IUD is now said to be small, except in those women who have a sexually transmitted disease (particularly chlamydia), at the time that the IUD is inserted. One way to evaluate the risk of IUDs in this regard is to study the pregnancy rates of women who have had IUDs in place as a birth control method, after removal. If IUDs are indeed associated with a high risk of pelvic inflammatory disease generally, then these pregnancy rates should be reduced as compared to controls. This has not been the case, generally, after IUDs are removed; women who have had them are able to get pregnant at the same rates as women the same age who have not had IUDs.[12]
References
- ↑ How Effective are IUDs from Planned Parenthood.
- ↑ IUD, an overview of IUD's from Planned Parenthood.
- ↑ American College of Obstetricians and Gynecologists (2011). "ACOG Practice Bulletin No. 121: Long-acting reversible contraception: Implants and intrauterine devices.". Obstet Gynecol 118 (1): 184-96. DOI:10.1097/AOG.0b013e318227f05e. PMID 21691183. Research Blogging.
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedStenchever - ↑ Grimes DA (2000) Intrauterine device and upper-genital-tract infection. Lancet 356:1013-9 PMID 11041414
- ↑ Prema K, Lakshmi BA, Babu S (1980) Serum copper in long-term users of copper intrauterine devices. Fertil Steril 34:32-35 PMID 7398904
- ↑ Cheng L et al. (2000) Interventions for emergency contraception. Cochrane Database Syst Rev CD001324 PMID 15266446
- ↑ Barrett S, Taylor C (2005) A review on pelvic inflammatory disease. Int J STD AIDS 16:715-20 PMID 16303062
- ↑ Wong AY, Tang LC, Chin RK (2010). "Levonorgestrel-releasing intrauterine system (Mirena) and Depot medroxyprogesterone acetate (Depoprovera) as long-term maintenance therapy for patients with moderate and severe endometriosis: a randomised controlled trial.". Aust N Z J Obstet Gynaecol 50 (3): 273-9. DOI:10.1111/j.1479-828X.2010.01152.x. PMID 20618247. Research Blogging.
- ↑ Bahamondes MV, Monteiro I, Castro S, Espejo-Arce X, Bahamondes L (2010). "Prospective study of the forearm bone mineral density of long-term users of the levonorgestrel-releasing intrauterine system.". Hum Reprod 25 (5): 1158-64. DOI:10.1093/humrep/deq043. PMID 20185512. Research Blogging.
- ↑ Greiner CU, Brune K, Haen E (2009). "Osteoporosis in a young woman after 6 years of levonorgestrel administration from intrauterine devices?". BMJ Case Rep 2009. DOI:10.1136/bcr.07.2008.0484. PMID 21686786. PMC PMC3030178. Research Blogging.
- ↑ Delbarge W et al. (2002) Return to fertility in nulliparous and parous women after removal of the GyneFix intrauterine contraceptive system. Eur J Contraception Reprod Health Care. 7:24-30 PMID 12041861
- Tadesse E (1996) Return of fertility after an IUD removal for planned pregnancy: a six year prospective study. East African Med J 73:169-71 PMID 8698014
- Chi I (1993) What we have learned from recent IUD studies: a researcher's perspective. Contraception 48:81-108 PMID 8403915