Molluscum contagiosum
| Molluscum Contagiosum Virus | ||||||||
|---|---|---|---|---|---|---|---|---|
 | ||||||||
| Scientific classification | ||||||||
|
Introduction
Molluscum Contagiosum Virus was first described and later it was named by Bateman in the early nineteenth century.[1] Over time, there was more cases that were described and similar to this virus, and overtime there was more and more information gathered on this. Goodpasture later described the similarities of molluscum and vaccinia.[2] Molluscum Contagiosum Virus is a poxvirus, which is a member of the family Poxviridae. Poxvirus are viruses that can be a family that infect both vertebrate and invertebrate animals. Molluscum contagiosum is a viral infection that seems to cause lots of papules or nodules on the skin. This disease it thought to infect humans only, but there has been cases where they found animals with Molluscum Contagiosum. This virus is said to be most common in children, but is found in sexually active adults, and those that are not immune. It is found worldwide with an increase in tropical areas. This disease is more prominent in areas, populations, institutions and communities with overcrowding, very bad hygiene, and high rate of poverty.They look like pimples with a pinkish, waxy, ugly look and a central pit, which can grow anywhere on an infected person.
Description and Significance
There are various types of Molluscum Contagiosum Virus, and they are most commonly seen on humans, but have been found to be on animals such as chickens, horses, oxen, cows, etc. As said, this is often seen on children and if on adults its due to sexually activity with an infected person. This virus is very contagious that can spread by contact with infected individuals or by association with fomites. Fomites are infected clothes, toys, towels, etc. It is found that there has been an increase of this disease mainly as a sexually transmitted disease, and seen that it is particularly rampant as a result of HIV (human immunodeficiency virus) infection. It is estimated to be between 5% to 20% of patients with HIV have symptoms of MCV. [3]
Taxonomy
To explain this further, Molluscum Contagiousum is a poxviruses from the family of Poxviridae. There are four genera, which are Orthopox, Parapox, Yatapox, and Molluscipox. Molluscipox gives rise to the virus Molluxcum Contagiosum. The name for Poxviridae viruses comes from the original grouping of the virus related with the disease that produced poxes on the skin. The subfamily is Chordopoxvirinae, with the Genus Molluscipoxvirus, and the species being MCV.
Types of Viruses for each genera: Orthopox: variola virus, vaccinia virus, cowpox virus, monkeypox virus, smallpox ; Parapox: orf virus, pseudocowpox, bovine papular stomatitis virus; Yatapox: tanapox virus, yaba monkey tumor virus; Molluscipox: molluscum contagiosum virus (MCV).[4] There are four main subtypes of molluscum contagiosum: MCV I, MCV II, MCV III, and MCV IV. All subtypes cause similar clinical lesions in genital and nongenital regions. Studies show MCV I to be more prevalent (75%–90%) than MCV II, MCV III, and MCV IV, except in immunocompromised individuals.[5]
Genome Structure
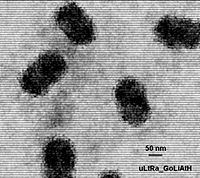
[6]. By the collaboration of information from experiments conducted over the years by Tatiana G. Senkevicha, Eugene V. Kooninb, Joachim J. Bugertc, a, Gholamreza Daraic and Bernard Mossa and various other scientists, we discovered that the Molluscum Contagiosum Virus is a non-segmented molecule of single double-stranded linear DNA with 180,000 to 200,000 nucleotides.It is said that there are 163 genes identified which encode 182 proteins. Among those, 105 proteins are counterparts in OPV (''Orthopoxviruses''). The OPV protein are considered to be the essential proteins for replication, and is noted that these proteins are highly conserved in MCV when undergoing transcription. There are twenty MCV proteins with OPV counterparts that have their own homologs, and some even have their own functional motifs. Despite other factors, the physical order and regulation of essential ancestral poxvirus genes have been largely conserved in these MCV's and OPV's. [7]The picture on the left is a table of Genomic information on various viruses.
They are usually complex structure and is consistent with the structure of poxviruses, with an envelope, core, surface membrane, and lateral bodies, and which contains infections in their envelope. The virons are in diameter of 200nm-300nm in length.[8]
Prevention
Since we already know its a contagious disease, we should be careful to avoid being in contact with someone who is infected. No sharing of clothes, towels, or any physical contact. Adolescents and adults who have MCV is due to sexual contact, so being careful and aware of this should be in care of mind. And definitely, being clean and have good hygiene can keep one from getting this disease. It was found that swimming pool may facilitate the spread of molluscum contagiousum through fomites. Steer clear of steam baths, saunas, and communal spray baths have also been found that it may help in transmission.
Symptoms
Molluscum causes pimple-like bumps on skin. There is not really any pain or discharge, but can be itchy and blisterish like to some individuals. They are nasty looking pinkish, yellowish bumps on the skin. They can look like small, waxy, raised polyp-like growths. They can be white, yellow, clear, or pinkish. Usually, at first we see one papule on our skin, and then from that they multiply and spread. Few individuals get MCV being red scaly skin with blisters around it.
Treatment
There are various ways to treat Molluscum Contagiosum. In most cases, this is not a serious case of disease that doesn't harm any organs and such. This disease if taken caution upon finding out can be treated pretty quickly. The issue with molluscum contagiosum is that the individual tends to pick and scratch at it causing more inflation, and risking a wider range of skin being infected. Some methods of treatment are putting on creams or having it surgically removed, etc. Few of the methods mentioned are cryosurgery(freezing the lesion with liquid nitrogen), evisceration, curettage(the piercing of the core and scraping of caseous or cheesy material), podophyllin and podofilox, Imiquimod, and cantharidin(a blistering agent usually applied in an office setting) as well as others. The most common method till recently was using a cream named Imiquimod(T cell modifier), which you apply four weeks nightly, resulting in the clearing of it in three months, and if you want it removed faster than that one would have a pulsed dye laser, which has been documented with excellent results. The therapy was well tolerated, without scars or pigment anomalies. The lesions resolved without scarring at 2 weeks. Studies show 96%–99% of the lesions resolved with one treatment.[9] The pulsed dye laser is quick and efficient, but its quite expensive which makes people look for other means. Though as of lately researching this, its seems most patients are using Cantharidin for treatment.
Recent research
- Efficacy of Cantharidin in Molluscum Contagiosum- to see the success rate of the treatment of Molluscum Contagiosum on patients.[10]
- The Incidence of Molluscum contagiosum among American Indians and Alaska Natives. Tells us of their findings regarding this molluscum and its the gathered data from this population and how it relates to population in general. [11]
- Parental Satisfaction, Efficacy, and Adverse Events in 54 Patients Treated With Cantharidin for Molluscum Contagiosum Infection. This study was conducted to record and analyze the efficacy, tolerability, and parental satisfaction of cantharidin in a patient population.[12]
Reference
- ↑ Bateman F. Molluscum contagiosum. In: Shelley WB, Crissey JT, eds. Classics in Dermatology. Springfield IL; Charles C Thomas, 1953, p20.
- ↑ Bretz S. Molluscum Contagiosum. Emedicine Journal April 25,2001;2(4).http://dermatology.cdlib.org/92/reviews/molluscum/diven.html#1
- ↑ 1. Billstein SA. Mattaliano VJ Jr. The "nuisance" sexually transmitted diseases: Molluscum contagiosum, scabies, and crab lice. Med Clin North Am 1990; 74: 1487-1505. 2.Schwartz JJ. Myskowski PL: Molluscum contagiosum in patients with human immunodeficiency virus infection. J Am Acad Dermatol 1992;27:583. 3. Lombardo PC. Molluscum contagiosum and the acquired immunodeficiency syndrome. Arch Dermatol 1985; 121: 834-835.http://dermatology.cdlib.org/92/reviews/molluscum/diven.html#1
- ↑ Georg, Paul; Johannes Blümel, Reinhard Burger, Christian Drosten, Albrecht Gröner, Lutz Gürtler, Margarethe Heiden, Martin Hildebrandt, Bernd Jansen, Thomas Montag-Lessing, Ruth Offergeld, Rainer Seitz, Uwe Schlenkrich, Volkmar Schottstedt, Johanna Strobel, Hannelore Willkommen, and Carl-Heinz Wirsing von König (December 2010). "Orthopox Viruses: Infections in Humans". Transfus Med Hemother 37 (6): 351–364. DOI:10.1159/000322101. PMC3048946. Retrieved on 16 October 2013. Research Blogging.
- ↑ Gottlieb SL, Myskowki PL. Molluscum contagiosum. Int J Dermatol 33: 453-461,1994. Yamashita H, Uemura T, Kawashima M. Molecular epidemiologic analysis of Japanese patients with molluscum contagiosum. Int J Dermatol 1996;35:99-105.
- ↑ Etten, James L. Van (2002) http://www7.nationalacademies.org/ssb/nanopanel2vanetten-1.gif
- ↑ Tatiana G. Senkevicha, Eugene V. Kooninb, Joachim J. Bugertc.Received 18 February 1997; revised 26 March 1997; accepted 15 April 1997. ; Available online 12 April 2002. http://www.sciencedirect.com/science?_ob=ArticleURL&_udi=B6WXR-45K15Y8-6D&_user=10&_rdoc=1&_fmt=&_orig=search&_sort=d&view=c&_acct=C000050221&_version=1&_urlVersion=0&_userid=10&md5=54d0c349fe732cbe9bf360a3a8090d03#bm4.1
- ↑ Hazelton, Paul R.; Hans R. Gelderblom (March 2003). "Electron Microscopy for Rapid Diagnosis of Emerging Infectious Agents". Emerg Infect Dis 9 (3): 294–303. DOI:10.3201/eid0903.020327. PMC2958539. Retrieved on 16 October 2013. Research Blogging.
- ↑ Daniel Hanson and Dayna G. Diven. Dermatology Online Journal 9(2): 2. http://dermatology.cdlib.org/92/reviews/molluscum/diven.html#1
- ↑ http://clinicaltrials.gov/ct2/show/NCT00667225
- ↑ http://www.find-health-articles.com/rec_pub_19381289-the-incidence-molluscum-contagiosum-american-indians-alaska-natives.htm
- ↑ http://cpj.sagepub.com/cgi/content/abstract/48/2/161?rss=1