Potassium in nutrition and human health
To maintain health, the diet of humans must contain potassium, in its ionic form (K+), usually as potassium salts of organic acids in food (e.g., potassium citrate). In 2004-2006, the Institute of Medicine of the National Academies of Science[1] and its Food and Nutrition Board[2] recommended that adult humans consume 4700 milligrams (mg) of potassium per day, which, calculated from the atomic mass of potassium (39.1 mg per mmol), amounts to 120 millimoles (mmol) potassium per day: 4700 mg/39.1 mg/mmol =120 mmol. That intake of potassium substantially exceeds estimates from recent surveys of average intakes by the general population. Subsequent sections will discuss potassium intake recommendations for children and special groups.
Introduction
Potassium ranks as the most abundant cation (positive ion) inside animal cells (intracellular), and as such contributes critically in numerous important ways to the optimal functioning of cells and therefore to optimal functioning of the organ systems and individuals they compose. Among other metabolic functions, potassium plays a role in the synthesis of proteins and in the biochemical transformations required for carbohydrate metabolism.
The ratio of the concentrations of potassium in intracellular fluid (ICF) to that in the cells' surrounding extracellular fluid (ECF) has important effects on the rate of transmission of electrical activity (pulses) along nerve fibers and skeletal muscle cells, which, among other things, affects the degree of contraction of the smooth muscles of arteries and arterioles (vascular tone). Inasmuch as extracellular potassium varies in the 3-6 mmol/L range, while intracellular potassium concentrations average about 145 mmol/L, small changes in extracellular potassium concentration have a greater effect on the ICF-to-ECF potassium concentration ratio than small changes in intracellular potassium concentration. Subsequent sections discuss the implication of changes in the ICF-to-ECF potassium concentration ratio in human physiology.
In healthy persons whose daily consumption of potassium does not vary greatly, the amount of potassium consumed equals the amount excreted, by the kidney and gastrointestinal tract predominantly. Physiologists refer to that equality as zero net external body potassium balance.
Disturbances relating to body potassium deficiency may result from:
- inadequate consumption of potassium-containing foods;
- inappropriate excretion of potassium in urine;
- inappropriate excretion of potassium in feces.
Disturbances relating to body potassium excess may result from:
- drugs and kidney diseases that impair the kidney’s ability to excrete potassium in urine;
- deficiency of hormones that act to promote kidney and gastrointestinal excretion of potassium.
Subsequent sections will elaborate on the above concepts.
Requirements for Potassium Consumption by Humans
Humans must regularly consume potassium because the body does not store it (as it does iron and fat, say), while the kidney continues to excrete it in the urine even when potassium intake ceases. Potassium-rich foods include leafy green vegetables, vine fruits (e.g., squash, tomatoes, cucumbers, etc.), root vegetables, and tree fruits (see below).
The Institute of Medicine of the National Academies of Science[1] and its Food and Nutrition Board[2] recommend as "Adequate Intake" (AI)[3] of potassium, in mmol/day, as 77 and 97 for children ages 1-3 and 4-8 years, respectively, and as 115 and 120 for children 9-13 and 14-18 years, respectively. For adult men and women, ages 19 to >70 years, they recommend an AI of potassium as 120 mmol/day, and the same amount for pregnant women as young as 14 years, increasing to 130 mmol/day for lactating women.
The Institue of Medicine claims:
"The AIs for potassium are based on a level of dietary intake that should maintain lower blood pressure levels, reduce the adverse effects of sodium chloride intake on blood pressure, reduce the risk of recurrent kidney stones, and possibly decrease bone loss." [1]
The claim reflects concerns about inadequate potassium consumption as contributing to hypertension (abnormally high arterial blood pressure), to facilitating dietary sodium chloride ('salt') intake's in contributing to hypertension, and to kidney stone and osteoporosis (soft, fracture-prone bones). This article will address those and other health-related effects of inadequate potassium intake in ore detail in later sections.
Potassium Content of Foods
Understanding the biological effects of dietary potassium ions (cations) requires an understanding of the nature of the negatively charged ions (anions) that accompany potassium in foods, balancing potassium’s positive charge, thus maintaining electroneutrality. In natural diets not subjected to commercial processing that includes addition of potassium salts—typically potassium chloride—a variety of organic anions (e.g., citrate, fumarate) accompany the potassium ions in foods, in amounts sufficient to nearly balance the positive charge of the potassium ions (i.e., in near chemical equivalent amounts). Following their absorption by the gastrointestinal tract, the body converts a large fraction of them to bicarbonate (an acid-neutralizing substance, or base), as an end-product of metabolism. Thus, diets with differing amounts of potassium exert potassium-induced biological effects associated and often interacting with the effects of the differing amounts of acid-neutralizing base, bicarbonate, as generated by the body from the potassium-accompanying organic anions. Physiologists often cannot dissect out the specific effects of the co-ions potassium and bicarbonate, when, for example, a person increases their dietary intake of potassium-rich foods, which typically contain bicarbonate-generating organic anions in abundance (see Table 1 and accompanying text).
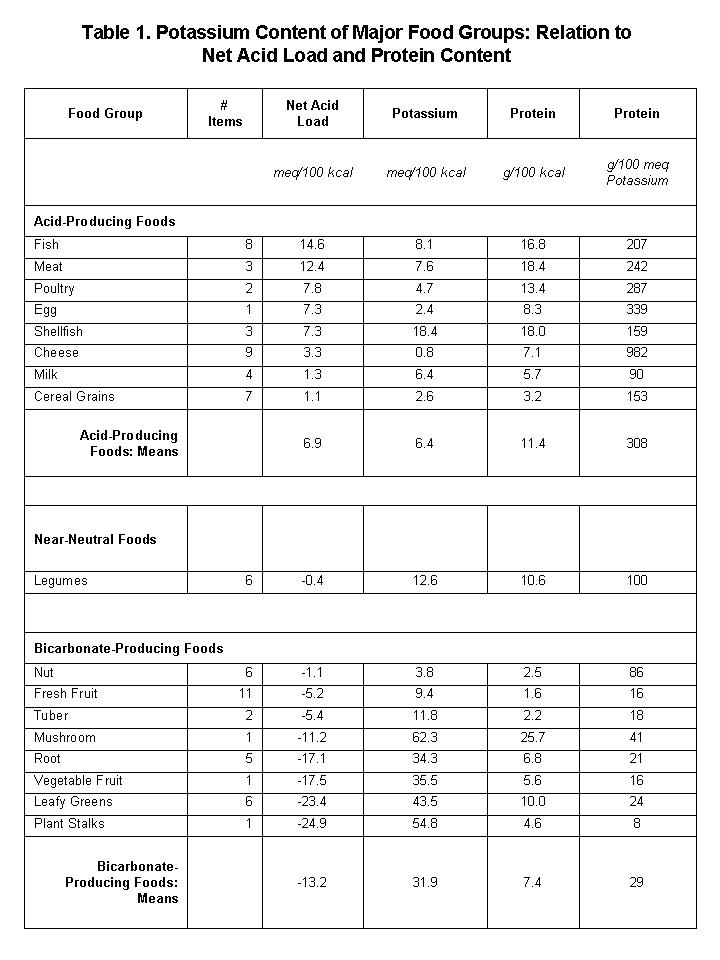
Table 1 shows the potassium content of the major food groups, indicating the relation of potassium content to the net acid (or bicarbonate) load supplied to the body by each food group (see comments following table). [NB: Bcause potassium ions have a single charge (univalent), 1 millimole (mmol) of potassium equals 1 milliequivalent (meq) of potassium.]
In Table 1, positive (+) and negative (–) values of net acid load represent acid-producing and bicarbonate-producing equivalents, respectively, in the units specified. Values of net acid load: calculated first for individual food items then averaged per food group, as per compositional values in:[4]. Acid load calculations: as described in:[5] Note that net acid-producing foods tend to have much higher ratios of protein-to-potassium than do net bicarbonate-producing foods (regression of net acid load against Protein/Potassium, r=0.48, p=0.05). Note the relatively low values of protein and potassium in the cereal grain group, of which whole grains comprised six of the seven items in the group.
Table 1 reveals a number of important aspects of food potassium:
- Per unit energy content (kilocalories, abbrev: kcal), non-cereal-grain plant foods provide the most abundant source of potassium.
- The top five plant-food sources of potassium (meq/kcal): root vegetables (celeriac, rutabaga, turnips, carrots, parsnips, sweet potato, potato, yams, onions); vegetable fruit (aka vine fruit) (tomatoes, zucchini, eggplant, cucumbers); leafy greens (spinach, lettuce, kale, chard); stalks (celery, broccoli stalks); mushrooms (not strictly a plant).
- The food sources richest in potassium also supply bicarbonate to the body, as indicated by negative values of "net acid load".
- The potassium content in acid-producing foods (animal-source foods and cereal grains) average about one-fifth that of plant-source foods, which do not contain sufficient quantities of bicarbonate-generating organic anions to neutralize the acid generated from protein and other sustances they contain.
- The ratio of protein-to-potassium in plant-source foods falls short of animal-source foods by a factor of 10.
- Legumes provide moderate amounts of potassium with little or no acid or bicarbonate load.
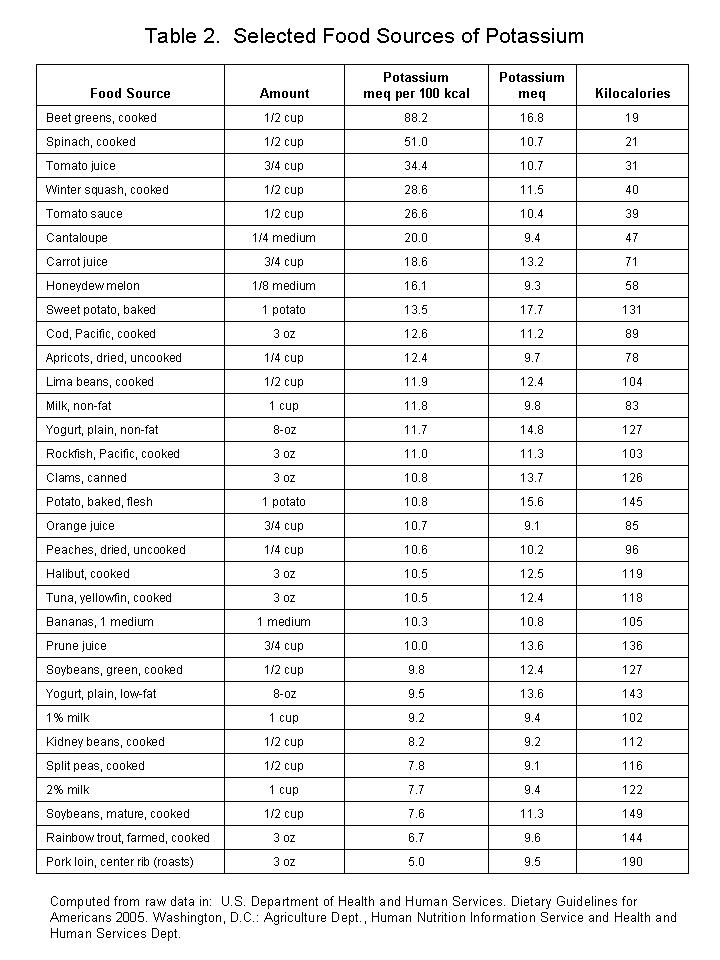
Table 2 lists selected food sources of potassium, showing amounts of potassium for standard portions, in descending order of amount of potassium per 100 kilocalorie of food source. Raw data for the calculations: taken from [6]
[...in progress...]
Potassium Intake, Blood Pressure Regulation, and Risk of Heart Disease and Stroke
Intervention-type research in humans has found that increasing potassium intakes reduces blood pressure in the arteries[7] [8] In both the population at large and in people with “high blood pressure” (aka “hypertension”), increasing potassium intake by 30-60 meq/day within the range of low (e.g., 30 meq/day) to high (e.g., 200 meq/day) intakes——either from food or prescribed supplements——tends to lower blood pressure.[9] The degree of blood pressure-lowering depends on a variety of factors, including amount of increase in potassium intake and ancestry.
Because people with higher blood pressures have greater risks of death from heart disease (e.g., heart attacks) and stroke (blockage or leakage of blood vessel in the brain),[10] dietary potassium’s effect in helping keep blood pressures lower in part justified setting the recommended intake of potassium at 120 meq/day---substantially higher than the population average---for American adults by the Institute of Medicine in 2005.[11]
These correspondences in part helped justify the Institute of Medicine’s recommendation to American adults to increase their intake of potassium to 120 meq/day:
- Higher potassium intakes reduce stroke risk independent of blood pressure[14].
The IOM makes no statement whether 120 meq/day potassium intake ‘’optimizes’’ cardiovascular health, but it sets no upper limit restrictions on potassium intake from food, which could reach 200-300 meq/day. Diets that potassium-rich include diets emphasizing the available abundant variety of potassium-rich vegetables and fruits, and deemphasizing fatty animal-source foods (like fatty hamburger meat) and high-fat-or-high-refined-carbohydrate foods with little-or-no additional nutrient content (like vegetable oil or pancake syrup)—diets considered health-fostering in many ways besides mitigating high blood pressure tissue injury.
Research has not determined optimal potassium intake ranges for maximal protection against heart disease and stroke and other detrimental effects of hypertension.
Dietary Potasium and Risk of Osteoporosis
[...in progress...]
Dietary Potassium and Risk of Kidney Stones
[...in progress...]
References
- ↑ 1.0 1.1 1.2 Otten JJ, Hellwig JP, Meyers LD (editors) 2006) Dietary Reference Intakes: The Essential Guide to Nutrient Requirements. National Academies Press. Pages 370-379. ISBN 0-309-65646-X
- ↑ 2.0 2.1 Panel on Dietary Reference Intakes for Electrolytes and Water. Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. Food and Nutrition Board. Institute of Medicine of The National Academies (2004) Dietary Reference Intakes For Water, Potassium, Sodium, Chloride, and Sulfate “Potassium” pp. 186-268. The National Academies Press, Washington, D.C.
- ↑ Note:*The Food and Nutrition Board of the U.S. Institute of Medicine establishes values for “Adequate Intake” (AI) for nutrients when insufficient data precludes establishing a “Recommended Dietary Intake” (RDA) for that nutrient. It bases AI values how much of the nutrient a group (or groups) of apparently healthy people consume, as determined by observation or experiment. Determination of AI values requires judgments of state of health, in particular in reference to the nutrient’s health effects.
- ↑ Souci SW, Fachmann W, Kraut H. (2000) Food Composition and Nutrition Tables. Stuttgart, Germany: Medpharm GmbH Scientific Publishers
- ↑ Sebastian A, Frassetto LA, Sellmeyer DE, Merriam RL, Morris RC, Jr. (2002) Estimation of the net acid load of the diet of ancestral preagricultural Homo sapiens and their hominid ancestors. American Journal Clinical Nutrition 76:1308-16
- ↑ U.S. Department of Health and Human Services. Dietary Guidelines for Americans 2005. Washington, D.C. Agriculture Department, Human Nutrition Information Service and Health and Human Services Department
- ↑ 7.0 7.1 Cappuccio FP, MacGregor GA. (1991) Does potassium supplementation lower blood pressure? A meta-analysis of published trials. ‘’J Hypertens’’ 9:465-73
- ↑ 8.0 8.1 Whelton PK, He J, Cutler JA, Brancati FL, Appel LJ, Follmann D, Klag MJ. (1997)Effects of oral potassium on blood pressure. Meta-analysis of randomized controlled clinical trials. ‘’JAMA’’ 277:1624-32
- ↑ Cite He MacGregor Others
- ↑ van den Hoogen PCW, Feskens EJM, Nagelkerke NJD, Menotti A, Nissinen A, Kromhout D, The Seven Countries Study Research Group. (2000) The Relation between Blood Pressure and Mortality Due to Coronary Heart Disease among Men in Different Parts of the World. ’’The New England Journal of Medicine’’ 342:1-8 [[https://content.nejm.org/cgi/content/full/342/1/1/ Abstract and Full-Text Here
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs nameddri06 - ↑ Hansen TW, Jeppesen J, Rasmussen S, Ibsen H, Torp-Pedersen C. (2005) Ambulatory Blood Pressure and Mortality: A Population-Based Study. ‘’Hypertension’’ 45:499-504
- ↑ van den Hoogen PCW, Feskens EJM, Nagelkerke NJD, Menotti A, Nissinen A, Kromhout D, The Seven Countries Study Research Group. (2000) The Relation between Blood Pressure and Mortality Due to Coronary Heart Disease among Men in Different Parts of the World. The New England Journal of Medicine 342:1-8 [[https://content.nejm.org/cgi/content/full/342/1/1/ Abstract and Full-Text Here
- ↑ Khaw K-T, Barrett-Connor E. (1987) Dietary potassium and stroke-associated mortality. A 12-year prospective population study. N.Engl.J.Med. 1987;316:235-40